MA Forms & MA Services
SpEd Forms’ MA Forms and MA Services help schools capture every eligible Medicaid reimbursement while complying with DHS requirements. By streamlining documentation and reducing errors, our tools make it easier for providers to document services accurately and for districts to recover valuable revenue, without adding extra administrative burden.
Why Choose MA Forms & MA Services
Effortless Documentation
Our MA Forms are directly connected to student IEPs, making documentation faster and more accurate. Service details flow seamlessly from the IEP to our MA Forms, reducing duplicate work and errors. This integration saves staff valuable time, makes providers’ day-to-day easier, and ensures the correct documentation backs every claim.
Optimized Reimbursements
We go beyond submitting claims—our tools and services help capture every eligible dollar. Detailed reports and an admin dashboard make it easy to track performance and catch issues early. With full-service billing, our expert team can manage the entire process, reducing denials and increasing reimbursements for your district.
Reliable Compliance
Protecting student information is at the core of what we do. Our platform is built to maintain confidentiality and fully supports HIPAA requirements, so sensitive data stays secure. With built-in compliance checks and audit-ready documentation, you can be confident your Medicaid billing meets all state and federal standards.

District Customization
Design your system to optimize your district’s unique needs and processes. With individual user permissions, site preferences, and MA Services tailored to you, SpEd Forms ensures that all eligible students and services are captured accurately. This flexibility gives your staff the confidence to work efficiently while keeping compliance and confidentiality at the forefront.

Powerful Tools
Easy-to-use interface with intuitive and flexible options for providers to document services for individuals or groups. Save hours on data entry using our CSV file import feature. Simply upload your file, and SpEd Forms will automatically generate MA claims, enhancing accuracy and reducing manual effort.
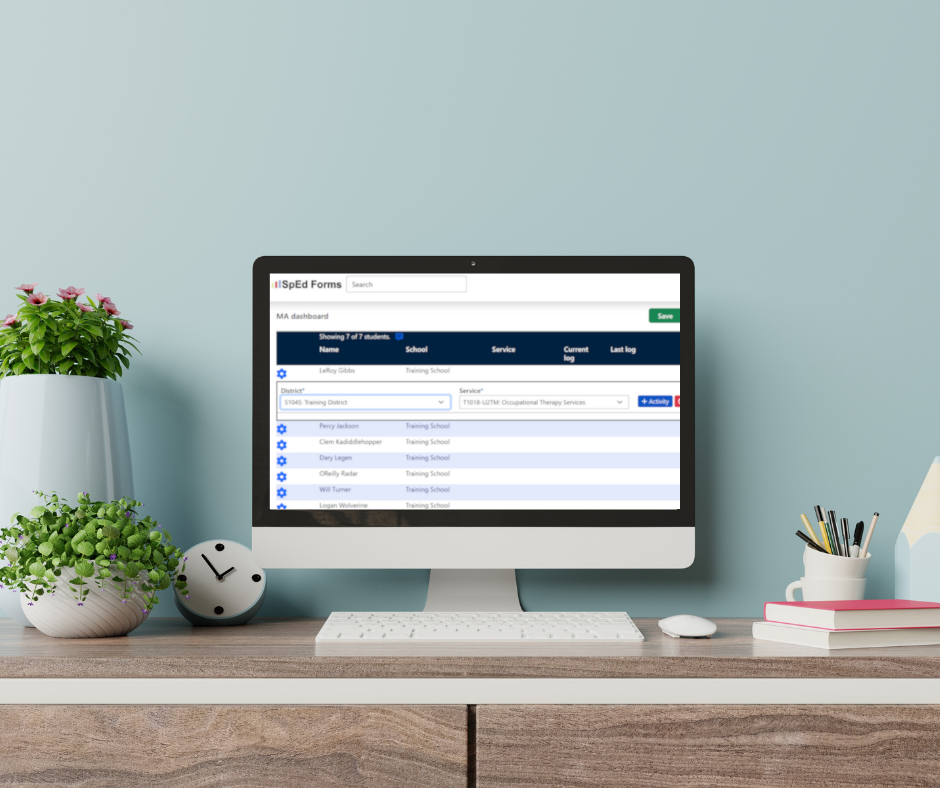
Claims Management
SpEd Forms takes the complexity out of Medicaid billing by managing the entire claims process from start to finish. From checking eligibility and claim submission to tracking, reconciliation, and re-billing, our system ensures every eligible service is captured and maximized for reimbursement. Built-in compliance monitoring helps your district align with both state and federal requirements.

Dedicated Support
We offer direct administrator and provider support for everything from rate adjustments to customized reporting and timely Medicaid program updates. During staffing transitions or coverage gaps, our interim billing services ensure claims continue to be processed seamlessly, protecting your revenue stream. We also provide hands-on assistance for audits, helping you maintain transparency and avoid costly penalties.